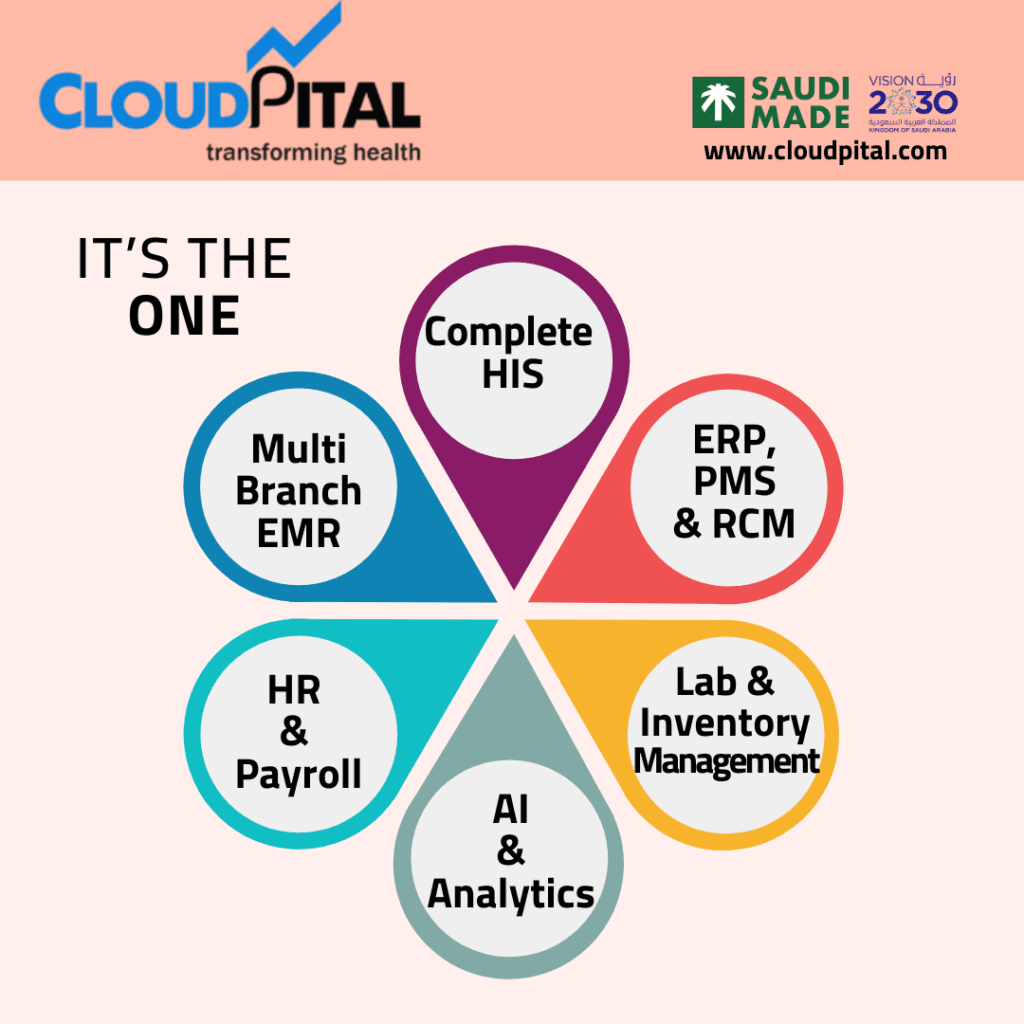
Cloudpital # 1 is one of the top RCM Revenue Cycle Management (RCM) is a crucial aspect of healthcare administration, encompassing the processes that healthcare providers use to manage the financial aspects of their services. A key function of RCM is to minimize claim denials, which can significantly impact a provider’s revenue and overall financial health. Claim denials can arise from various reasons, including errors in documentation, incorrect coding, lack of patient eligibility verification, and failure to meet payer requirements. By implementing effective RCM strategies, healthcare organizations can significantly reduce these denials and improve their financial performance. Here’s an in-depth look at how RCM can reduce claim denials in healthcare.
Click to Start Whatsapp Chatbot with Sales
Mobile: +966502737333
Email: sales@cloudpital.com
Cloudpital # 1 RCM
Improved Patient Registration and Eligibility Verification
One of the primary reasons for claim denials is incorrect patient information, particularly related to insurance eligibility. RCM can enhance this aspect through rigorous patient registration processes.
- Pre-Registration Verification: Before a patient’s visit, RCM can incorporate systems that verify insurance coverage. This may involve contacting insurance companies or using automated eligibility verification tools. Ensuring that a patient’s insurance is active and covers the proposed services can prevent many denials upfront.
- Accurate Data Collection: During registration, training staff to collect complete and accurate patient information—including demographics and insurance details—can mitigate errors. Implementing digital registration forms that guide users through necessary fields can further reduce mistakes.
Effective Coding Practices
Medical coding is a critical element of the claims process. Inaccurate coding is one of the leading causes of claim denials.
- Coder Education and Training: Regular training sessions for medical coders on current coding standards, payer-specific requirements, and updates to coding guidelines (like ICD-10 and CPT) can enhance accuracy.
- Utilization of Coding Software: Advanced coding software can assist coders in selecting the appropriate codes based on the documentation provided. This reduces human error and ensures that the correct codes are submitted.
- Auditing and Feedback Mechanisms: Implementing regular audits of coding practices allows organizations to identify patterns in errors and provide feedback to coders. This continuous improvement cycle can enhance the overall accuracy of submitted claims.
Comprehensive Documentation Practices
Robust documentation is vital for substantiating claims. Insufficient or unclear documentation often leads to denials.
- Standardized Templates: Creating standardized templates for clinical documentation can help ensure that all necessary information is captured consistently. This includes specific details about the diagnosis, treatment, and patient responses.
- Clinical Staff Training: Educating clinical staff about the importance of thorough documentation and what is required by payers can significantly improve the quality of records. This ensures that all treatments and services rendered are accurately captured.
- Real-time Documentation Support: Implementing systems that provide real-time support for documentation during patient encounters can ensure that clinicians do not overlook essential details that may lead to denials.
Payer-Specific Claim Submission Protocols
Different payers have unique requirements for claim submissions, and failure to adhere to these can result in denials.
- Knowledge of Payer Requirements: RCM teams should maintain updated knowledge of the specific requirements of various payers. This includes understanding different policies related to authorization, documentation, and coding.
- Customized Submission Processes: Developing customized claim submission processes for different payers can help ensure that all specific requirements are met before submission, thereby reducing the likelihood of denials.
- Regular Communication with Payers: Establishing strong relationships and regular communication with payers can facilitate quicker resolution of issues that may arise, as well as provide insights into payer trends that might affect claims.
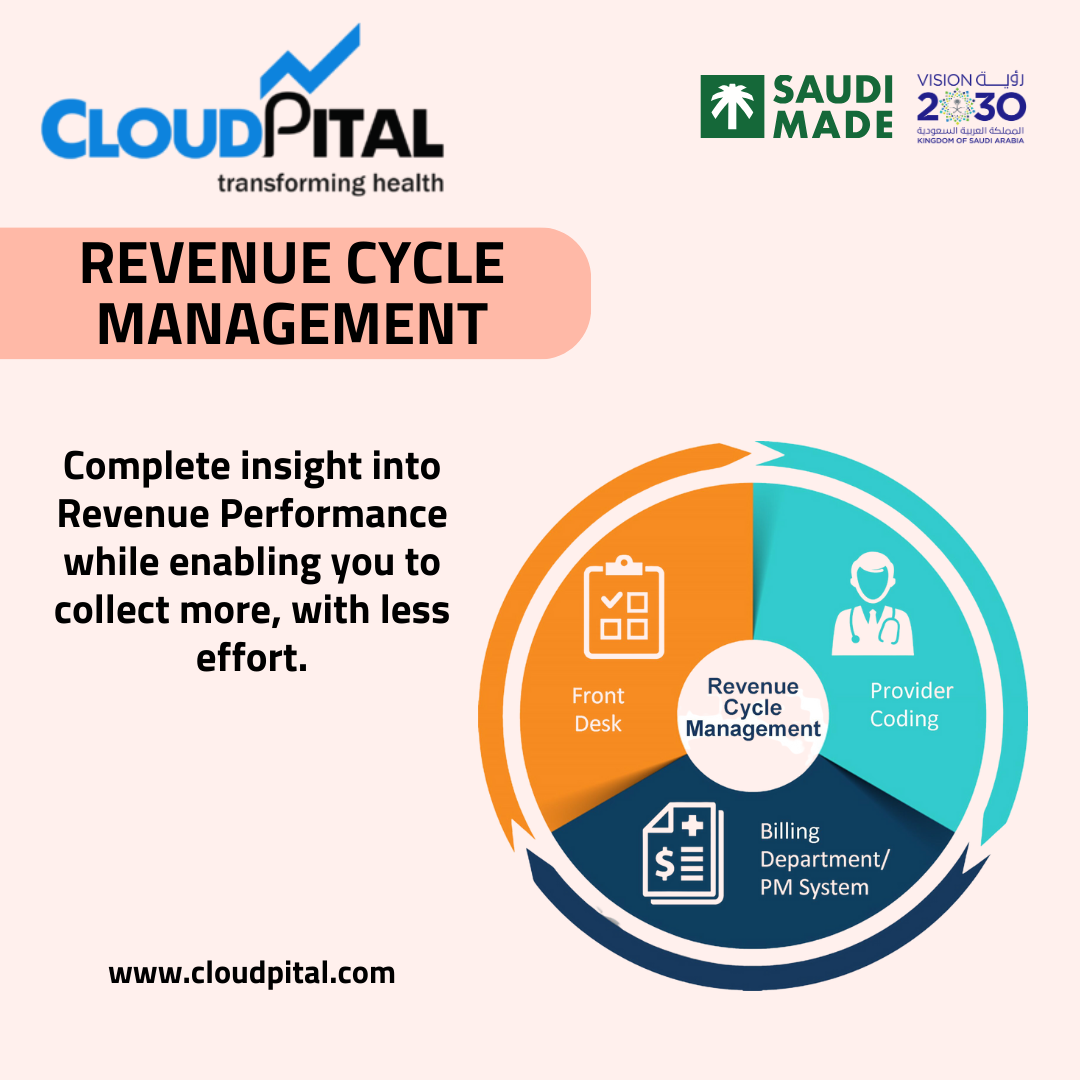
Timely Claims Submission
The timing of claims submissions is crucial in the Medical Solutions in Saudi Arabia. Delayed submissions can lead to missed deadlines, resulting in denials.
- Automated Claims Submission: Utilizing RCM software that automates the claims submission process ensures that claims are sent promptly after patient visits. Automation reduces the risk of human error and ensures compliance with submission timelines.
- Tracking and Monitoring Systems: Implementing systems to track claims from submission to payment can help identify delays and address issues proactively. This allows RCM teams to follow up on claims that have not been processed in a timely manner.
Denial Management Strategies
Even with the best practices in place, denials may still occur. Having a robust denial management strategy is essential.
- Denial Analysis: Analyzing denied claims to identify trends and root causes can provide valuable insights. Understanding why claims are denied—whether due to documentation issues, coding errors, or authorization problems—allows organizations to target specific areas for improvement.
- Appeal Processes: Establishing a clear and efficient appeals process can help recover denied claims. Training staff on how to craft effective appeal letters, including gathering supporting documentation, can improve the chances of overturning denials.
- Feedback Loops: Creating feedback loops between clinical staff, coding teams, and billing departments ensures that lessons learned from denied claims are communicated across the organization, facilitating ongoing improvements.
Patient Engagement and Communication
Engaging patients in the financial process can help minimize denials related to eligibility and understanding of benefits.
- Patient Education: Providing patients with clear information about their coverage and any potential out-of-pocket costs can help them understand their responsibilities. This knowledge can encourage them to verify their eligibility and avoid situations that might lead to denials.
- Transparent Financial Policies: Clearly communicating financial policies, including billing practices and payment expectations, can help set realistic patient expectations and prevent misunderstandings that could result in denials.
- Utilizing Patient Portals: Implementing patient portals that allow patients to access their information, verify coverage, and review bills can enhance engagement and reduce claims that are denied due to misinformation.
Utilizing Data Analytics
Data analytics play a crucial role in EMR Software in Saudi Arabia by providing insights that can help reduce claim denials.
- Identifying Trends: Analyzing claims data can help identify patterns in denials related to specific departments, procedures, or payers. This information can guide targeted training and process improvements.
- Predictive Analytics: Using predictive analytics can help organizations anticipate which claims are at risk of denial, allowing them to take corrective actions before submission.
- Benchmarking Performance: By comparing denial rates against industry benchmarks, healthcare organizations can gauge their performance and identify areas that need attention.
Conclusion
In conclusion, effective Revenue Cycle Management is essential for reducing claim denials in healthcare. By improving patient registration processes, enhancing coding practices, ensuring comprehensive documentation, and maintaining a proactive approach to payer requirements, healthcare organizations can significantly minimize denials. Furthermore, implementing robust denial management strategies, engaging patients in the financial process, and utilizing data analytics can create a culture of continuous improvement. Ultimately, by addressing the root causes of claim denials and fostering a streamlined RCM process, healthcare providers can enhance their financial stability and focus more on delivering quality care.
Click to Start Whatsapp Chatbot with Sales
Mobile: +966502737333
Email: sales@cloudpital.com
How can RCM reduce claim denials in healthcare? similar software solutions prices were updated on 2025-07-15T20:14:31+00:00 in Saudi Arabia in Mecca, Medina, Riyadh, Khamis Mushait, Yanbu, Jeddah, Dammam, Unaizah, Uqair, Ha’il, Ta if, Al Bahah, Dhahran, King Abdullah Economic City, Najran, Diriyah, Qatif, Khafji, Jubail, Abqaiq, List of Cities and Towns in Saudi Arabia, Ras Tanura, Turubah, Jazan Economic City, Knowledge Economic City, Medina, Khobar, Abha, Tabuk, Saudi Arabia, similar software solutions prices were updated on 2025-07-15T20:14:31+00:00 We also provide in Saudi Arabia services solutions company in Hafar Al-Batin, Udhailiyah, Al-Awamiyah, Hofuf, Hautat Sudair, Buraidah, Tayma, Duba, ‘uyayna, Saihat, Al-Kharj, Al-ula, Jizan, Rumailah, Ar Rass, Arar, Shaybah, Al Majma’ah, Rabigh, Dhurma, Haradh, List of Saudi Cities by Gdp Per Capita, Badr, Sudair Industrial City, Baljurashi, Shaqraa, Al-Khutt, Habala, Ad Dawadimi, Dawadmi, Layla, similar software solutions prices were updated on 2025-07-15T20:14:31+00:00 Price is SAR 100 and this was updated on updated on 2025-07-15T20:14:31+00:00 similar How can RCM reduce claim denials in healthcare? software solutions prices were updated on 2025-07-15T20:14:31+00:00 in Saudi Arabia in Haql, Afif, Al-Abwa, Farasan, Al-Jaroudiya, Thadig, Al-Thuqbah, Al Wajh, Almardmah, Al-Zilfi, Muzahmiyya, Prince Abdul Aziz Bin Mousaed Economic City, Tharmada’a, Skaka, Um Al-Sahek, Sharurah, Tanomah, Bisha, Dahaban, Al Qunfudhah, Qurayyat, Saudi Arabia, Ha’ir, as Sulayyil, Al Lith, Turaif, Al-Gway’iyyah, Samtah, Wadi Ad-Dawasir, Az Zaimah, Safwa City, Jalajil, Harmah, Mastoorah, Hotat Bani Tamim, Jabal Umm Al Ru’us, Rafha, Qaisumah, Al-Ghat, Hajrah, Al-Hareeq. Excerpt: Jeddah (also spelled Jiddah, Jidda, or Jedda; Arabic: Jidda) is a Saudi Arabian city located on the coast of the Red Sea and is the major urban center of western Saudi Arabia similar software solutions prices were updated on 2025-07-15T20:14:31+00:00 Price is SAR 100 and this was updated on updated on 2025-07-15T20:14:31+00:00
26-9-2024